The SAGE Guideline Model will
contain various attributes that will work together
to produce an effective means for encoding medical
guidelines:
Recommendation Sets - A subset of
guideline content tailored to the workflow, roles,
entities and actions within a specific healthcare
enterprise. When encoding the guideline for SAGE,
an enterprise team of clinical experts must interpret
the guideline statements and create one or more plans
that will support the guideline goals in the specific
work environment of their health care organization.
To achieve this, the recommendation set employs four
"nodes": Context, Decision, Action, and
Route.
1. Context Node- Specifies and
declares the assumptions made about the health care
enterprise work model that are otherwise implicit
in every instance of a guideline implementation;
their defining attributes specify their trigger
events, clinical setting, and patient state. For
example, a context node can specify that a physician
in an emergency department triggers the guideline
interaction by beginning an order entry session
and identifying the diagnosis as acute neurological
deficit.
2. Action Node- Models one or more
information system activities employed in support
of a recommendation set; they can include support
for messaging to system devices like Inbox reminders
or workstation reminders.
3. Decision Node- Describes the acquisition
of some data (directly from the patient EMR or interactively
by asking
the clinician) and the employment of a decision
model to evaluate branching logic.
4. Routing Node- Synchronizes multiple
activity paths.
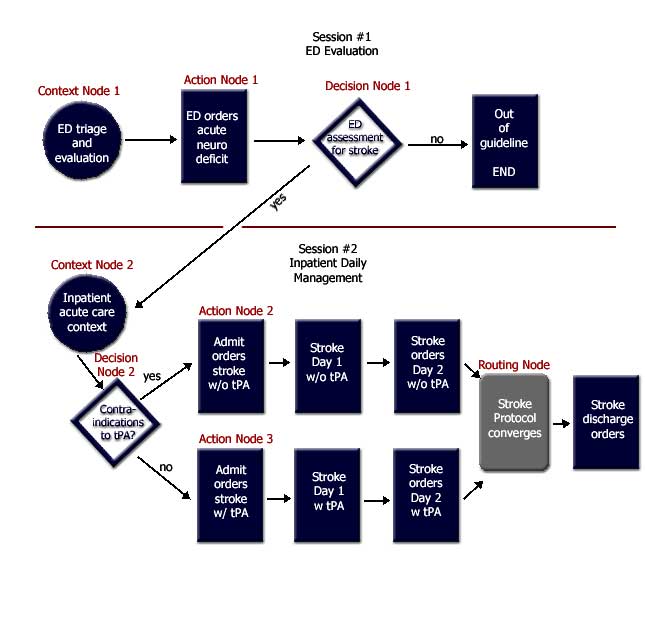
The graphic above represents a sample
recommendation set based on the guideline
from the Institute for Clinical Systems Improvement
(ICSI) for triage and treatment of acute ischemic
stroke. This guideline focuses upon rapid evaluation
of the patient with acute neurologic deficit, a
search for contra-indications to tissue plasminogen
activator (tPA), and administration of tPA to selected
eligible patients.
The recommendation set consists of
two sessions (set of one or more interactions between
user and SAGE/CIS symbiote). Context Node
1 specifies the context of an emergency
department physician triage examination, while Context
Node 2 depicts the inpatient physician
daily order sessions in the treatment of the stroke.
More specifically, Context Node 1 specifies that
a physician in the Emergency Department (ED) triggers
the guideline interaction by beginning an order
entry session and identifying the diagnosis as acute
neurologic deficit. Node 2 is triggered as the inpatient
physician initiates daily order sessions for management
of the patient admitted with a stroke diagnosis.
Action Nodes 1 - 3
model the use of order sets to be employed in the
stroke protocol. In the example above Action Node
1 is a protocol order set for rapid evaluation in
the emergency department. Action Nodes 2 and 3 contain
order set specifications for stroke admission orders
in the setting of treatment without and with tPA,
respectively. Since all context, action and decision
nodes may have associated scheduling constraints,
the execution sequence may be interrupted, with
explicit time management, as in the successive delivery
of Day 1 and Day 2 order sets in this example.
In Decision Node 1,
a user decision that the patient does not have a
stroke leads to exit from the guideline scenario.
In Decision Node 2, assessment of tPA contraindications
determines whether the patient is eligible for tPA.
Each decision node, in addition to scheduling features,
has two or more concluding states and a bound decision
model which may employ an argumentation structure,
a neural or Bayesian network, or other methods determined
by the needs of the guideline.
The Routing Node
in the example above is where the two care plans
merge ("with" or "without tPA"),
and both of the activity paths are synchronized
to the stage where the patient can be discharged.